This post was reviewed for medical accuracy by Rosalie Gunson, a Certified Registered Nurse Practitioner specializing in fertility care.
So far my posts have focused on getting pregnant, but there’s another group of people in the infertility world who need more support: those who struggle to stay pregnant. This post will focus on trying to conceive (TTC) with recurrent pregnancy loss (RPL).
Recurrent pregnancy loss is defined as two or more miscarriages before 20 weeks. Even if they were previously able to get pregnant without help, women with RPL may turn to fertility specialists to help them conceive again and hopefully make it to full-term with their rainbow baby.
Preparing to conceive a rainbow baby
Physically recovering from a recent loss
Before you can realistically think about another pregnancy, you need to physically heal from the most recent loss. How much recovery is involved depends partly on how far along you were.
Very early losses may not be very noticeable aside from some extra bleeding or cramping. If the pregnancy was more established, you may need medication (for example, misoprostol) or surgery (a D&C) to clear out the tissue.
A few weeks afterward, your doctor may have you take a pregnancy test to confirm that your hCG level has fallen back to normal.
Once your body has healed from the miscarriage itself and you’re no longer bleeding, you can theoretically start trying again as soon as you get your cycle back. That can take 6-8 weeks or longer.
Specific strategies to prepare to conceive again
Anyone who’s had recurrent losses should consider consulting with a reproductive endocrinologist (RE) and/ or a MFM (also called a perinatologist). These specialists can meet with you before you try to conceive again.
You’ll probably be sent for some tests. For example:
- Blood tests to check for certain conditions, including thyroid problems
- HSG to check for abnormalities in the uterus
- Karyotype testing (genetic testing of both parents)
- Genetic testing of the fetal tissue, if applicable
Your doctor may be able to identify a reason for your losses and figure out a strategy for TTC successfully the next time. For example:
- If you have a chronic disease, do what you can to stabilize your condition first. For instance, diabetic women should get their blood sugar well under control. Women with severe mental health conditions or substance abuse disorders should get appropriate treatment before trying to conceive again.
- If your previous losses were due to a chromosomal problem (either yours or your partner’s), you could consider using donor eggs and/or sperm next time. Doing IVF with pre-implantation genetic testing may also be an option.
- If a structural problem was discovered in your uterus via HSG, you may be able to have surgery to fix it (depending on the nature of the problem). Surrogacy may be an option as well.
- If you had an incompetent cervix, you could consider getting a cerclage early in your next pregnancy. A cerclage is basically a little stitch that helps keep your cervix closed in early pregnancy.
Emotional considerations
You may be physically ready before you are emotionally ready, though. Grief is a very personal thing. Some women and couples may feel ready for another baby soon after loss. Others may need to wait a year or more before trying again, if they ever do.
Take whatever time you need. Don’t let anyone tell you how quickly you need to “get over it” or “move on.” Don’t let anyone try to judge you for mourning an early loss (“at least you weren’t very far along”) or a loss after a successful birth (“at least you already have a child”).
If you think you want to TTC again but you need some support working through your grief, consider:
- Mindfulness meditation
- Individual or couples counseling
- In-person or online support groups
- Reading success stories — and only success stories.Speaking of success stories…

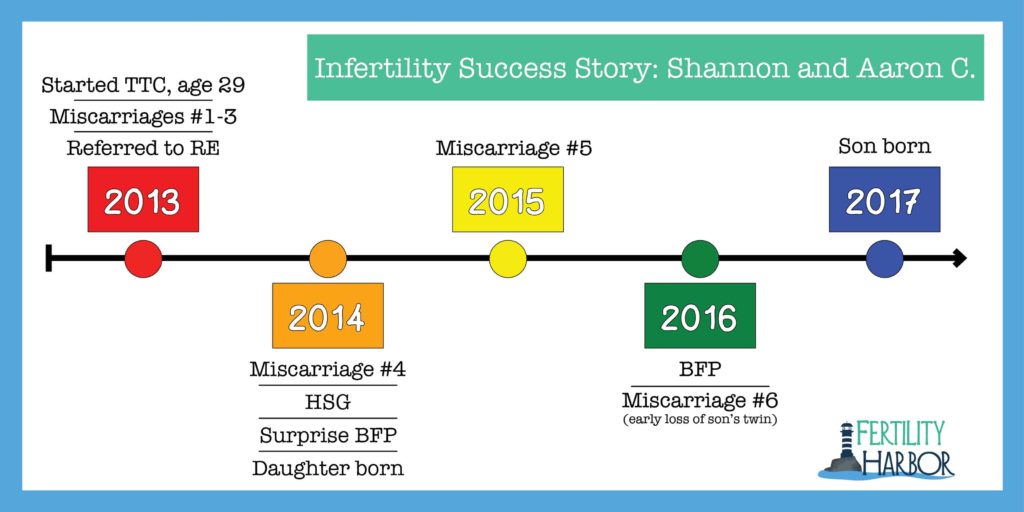
Infertility Success Story: Shannon and Aaron C.
Looking at this beautiful photo of my cousin Shannon with her family, you’d never guess that she had a long and painful journey to motherhood. She’s given me permission to share that journey here, although it’s complicated — I’ll have to simplify quite a bit!
Shannon and her husband, Aaron, had no problem getting pregnant — they were never even tested for male-factor fertility problems. But staying pregnant was another story.
Shannon had three miscarriages, all around 6 weeks, before she was referred to a reproductive endocrinologist. After a lot of testing, the RE diagnosed her with a MTHFR gene mutation and an immune issue that made her body see a developing embryo as a threat.
The RE helped her improve her body’s immune response with drugs such acyclovir and an intralipid infusion. She got another BFP on a Clomid cycle, but unfortunately the pregnancy was ectopic and had to be ended with methotrexate. That was miscarriage #4, and still no baby. As you can imagine, they were starting to lose hope.
They were relieved when an HSG showed no blockages or structural problems at all. About 6 weeks after the test, she went to a follow-up appointment and the scan revealed she was pregnant! She followed all the RE protocols and was able to stay pregnant this time.
That pregnancy wasn’t without complications, including a subchorionic hematoma and pre-eclampsia that required an emergency c-section around 37 weeks. But everyone was healthy, and the new parents were overjoyed to bring their rainbow baby home.
Shannon had one more early miscarriage (#5) before getting pregnant with her son. Tragically, her mom (my mom’s first cousin) passed away suddenly during the early weeks of that pregnancy.
Shannon found out that she’d originally been pregnant with twins, but only one continued to develop. She attributes the early loss of the second twin (#6) to her stress level at the time. Her son was born healthy as can be at 39 weeks via a scheduled c-section.
Given everything they went through, Shannon and Aaron have have decided that their family is complete!
Managing anxiety when you get pregnant again
After experiencing loss, your next pregnancy will inevitably feel different. You might find it hard to celebrate because you’re still bracing for bad news… but then you might feel guilty for not feeling sufficiently #blessed and #grateful. Or you might worry that getting excited about the new baby would somehow dishonor your angel babies.
Other signs of anxiety that might sound familiar to you:
- Over-analyzing every minor symptom, or worrying that you don’t feel pregnant enough
- Dreading ultrasounds and other tests because you’re afraid of the results
- Delaying telling family, friends, and co-workers about the pregnancy well past the customary 12 weeks
- Feeling superstitious about choosing names, planning a baby shower, or decorating a nursery before the baby is actually born
- Intense sadness around anniversaries, such as angel babies’ due dates
- Bursting into tears when someone asks if this is your first baby
Managing this anxiety can be difficult. Strategies that have worked for others include keeping busy with work, walking on the beach or in the woods, journaling, and celebrating the milestones along the way.
“I had a tough time being able to relax during my pregnancy with my daughter,” Shannon says. “Honestly, every time that I went to the bathroom and wiped, I expected to see blood. I was a member of quite a few support groups on Facebook, specifically those for women who were taking Lovenox during pregnancy and those who had MTHFR.”
“I remember reading a post about pregnancy after multiple losses and this really resonated with me: ‘Enjoy each milestone that you hit. Try not to think of your pregnancy as one big picture and celebrate each step no matter how little it may seem.’ This really helped me get through the days, but I was still a nervous wreck.”
“I’m sure that the woman who shared that piece of advice on that Facebook post a long time ago never realized the impact that her words would have on my life or the lives of others,’ Shannon says. ‘I think it’s so important to be there for each other, especially when it comes to adventures in infertility. You are not alone!'”
 Focusing on these sorts of mini-deadlines is a great way to keep yourself from being overwhelmed with anxiety about the big picture. In my 8 Tips for Staying Sane During Infertility/ IVF, a version of this idea is the very first tip.
Focusing on these sorts of mini-deadlines is a great way to keep yourself from being overwhelmed with anxiety about the big picture. In my 8 Tips for Staying Sane During Infertility/ IVF, a version of this idea is the very first tip.
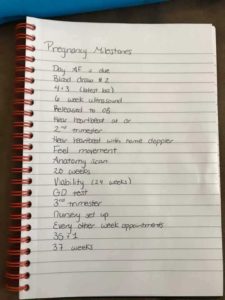
Another mama who suffered recurrent pregnancy loss wrote out a list of 18 milestones to focus on when she was TTC #2. I’m sharing it here with permission.
I love that she included dates that were uniquely meaningful to her. For example, her first child was born at 35+1, so she wanted to get at least that far with her second.
Common causes of pregnancy loss
I wanted to include some basic info about the common causes of miscarriage, but I didn’t want it to be triggering or distracting. That’s why I saved this section for the end.
What causes pregnancy loss before 12 weeks (an estimated 80% of all miscarriages)?
Most problems that lead to an early miscarriage are not predictable or avoidable — they stem from the fact that the fetus just wasn’t developing normally.
Here are a few common reasons for first-trimester pregnancy loss:
- Chromosomal defects in the fetus
- Blighted ovum (the fertilized egg never develops into a fetus)*
- Ectopic pregnancy (the fertilized egg implants in the wrong place, like the fallopian tubes)
- “Vanishing twin” (a twin pregnancy that spontaneously becomes a singleton pregnancy, usually so early that you wouldn’t have known it even happened without an internal ultrasound)*This is the reason my friend in the post TTC After a D&C had her D&C.
What causes pregnancy loss after 12 weeks?
The vast majority of pregnancy losses happen in the first trimester — often before women even know they were pregnant. Losses after 12 weeks are far less common.
Here are a few things that can cause pregnancy loss after 12 weeks:
- Multiples pregnancy (especially triplets or more)
- Structural defects in the fetus, especially in the brain or the heart
- Uterine abnormalities
- Complications from the mother’s chronic health condition (such as uncontrolled diabetes, thyroid disease, blood clotting disorder, etc.) or drug abuse
- Certain infections, including chlamydia and other STDs
- Problems with the placenta, such as placental abruption (when the placenta separates from the womb) or placental insufficiency (when not enough nutrients or oxygen get to the fetus)
- The umbilical cord getting knotted or squeezed
- Trauma to the abdomen (for example, from a car accident)
- Complications that require the baby to be born very prematurely, such as:
- Incompetent cervix (also called cervical insufficiency). This is when the cervix dilates too soon.
- Preterm Premature Rupture of Membranes (PPROM). This is when the water breaks too soon.
- Preeclampsia. This condition causes the mother’s blood pressure to be dangerously high and the only remedy is delivering the baby ASAP.
To infertility warriors who have experienced recurrent pregnancy loss:
I’m not going to say your heartbreak is inspiring,
because only a sociopath could be inspired
by such profound grief.
But your courage?
Your courage will move mountains, mama.
Further Reading:
“What is Recurrent Pregnancy Loss (RPL)?” — American Society for Reproductive Medicine (ASRM)
Resources for Grieving Parents:
Share Pregnancy & Infant Loss
March of Dimes
Still Standing Magazine
Stillbirthday
This post was last updated in March 2021.


 I’m Jenn! Here I am with my beautiful twin boys. My pregnancy was possible thanks to fertility treatment for PCOS.
I’m Jenn! Here I am with my beautiful twin boys. My pregnancy was possible thanks to fertility treatment for PCOS.


